Services
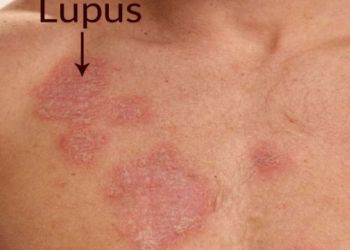
Systemic Lupus Erythematosus



What is SLE?
It is a systemic auto immune disease, in which the body’s immune system attacks the healthy cells of one owns body.
What causes it?
‘The Cause is ‘UNKNOWN’. But circulating immune complexes is a classical feature of SLE.
What happens in SLE?
It is one of the auto immune multi system disease in which the immune system is unable to differentiate between non self (e.g. an organism) and self (one’s own system). The major systems involved are Central Nervous system, kidneys, Blood vessels, heart, eyes, and skin, joints etc.
Is it curable?
SLE is an “INCURABLE DISEASE”, just like diabetes and hypertension. But with the recent availability of good treatment modality, SLE has very bright outlook as in diabetes and hypertension. With current treatment options, patients may feel ‘as if cured, but only with medications. Cure means normality without any medications & that does not happen in SLE. If you have any such belief, please remove that from mind. This misconcept often make patients stop treatment and get in to life threatening emergency.
What are the available treatment options and its duration?
Majority are treated with steroids. Patients who are on steroids need not get frightened, as the actions and side-effects are known to the physicians. Hence they can be monitored. The initial dosage of steroids is as high as 1 mg/kg/day which is tapered slowly after about 2 to 3 months and later to a maintenance dose.
Caution: Premature tapering of steroids is dangerous. Which may cause flare up of disease and ultimately, the patient will end up getting more steroid. So, seek a trained Rheumatologist. There are other second line immunosuppressants line Mycophenolate, Cyclophophamide & Azathioprine which help taper steroids. Remember- steroids are also produced in our own normal body
What is the most common expected side effects of steroids?
- Skin changes like stretch marks.
- Opacity of lens
- Increased blood pressure
- Increased blood sugar
- Low immunity leading to infections.
- Thin bone and fracture risk
What are the other drugs given for SLE?
Along with steroids, Chloroquine or hydroxy chloroquine are given, which has a mild steroid sparing effect. These drugs prevent Nervous system disease relapse, thrombosis and infection.
- There are 6 types renal involvement and treatments for each differ.
- Mycophenolate & Cyclophosphamide are the most effective treatment options for the worst type of kidney involvement (type III & type IV)
- To prevent fractures due to decrease bone density-Calcium tablets and vitamin D tablets are prescribed.
Should the patients take the drugs over the counter (OTC)?
No. Steroids have long term side effects. Tapering and monitoring should be done to minimize these effects. Hence care should be taken in not taking these drugs over the counter.
How frequently the doctor should be consulted?
After diagnosis, follow up should be made every month. Once stable the patient should visit the physician at-least once in 3 months. An eye check is a must once in 6 months. Any inter current infection should be treated promptly.
is there a role for diet restriction?
“No diet can cause or no diet can cure SLE”. But fish can be taken often, as it contains Omega 3 fatty acids, which has an anti-inflammatory effect and also prevents cardiac complications. Restrict saturated fat and high carbohydrate diet. Most Indian spices are beneficial especially curcumin in turmeric.
Is it hereditary?
Most systemic autoimmune diseases have multifactorial etiology and there is a likely hood of the off springs getting SLE or any other connective tissue disorders. But it doesn’t follow any inheritance pattern and often not predictable.
What are the concerns with pregnancy in a SLE patient?
Pregnancy flares up the disease leading to a higher risk of miscarriages due to the presence of Antiphospholipids antibodies. Pregnancy in SLE need special care as there is risk to the life of both mother and fetus, if not monitored well.
Is there any preventive drug for an STA patient who becomes pregnant?
No clear evidence in that; directing close monitoring with Rheumatologist/ immunologist and obstetrician is the best option. Blood thinners are also used under supervision.
